A well-rounded GME experience for the next generation of family health physicians.
Welcome to the Wellstar Kennestone Family Medicine Residency Program. I am honored to introduce you to our program and our big family.
Family medicine is a unique and rewarding field. We are committed to providing a supportive and nurturing environment where residents can thrive both personally and professionally. As you are about to start this exciting chapter of your medical career, we want you to know that you are joining a community that values collaboration, diversity, and a shared passion for delivering high-quality patient care.
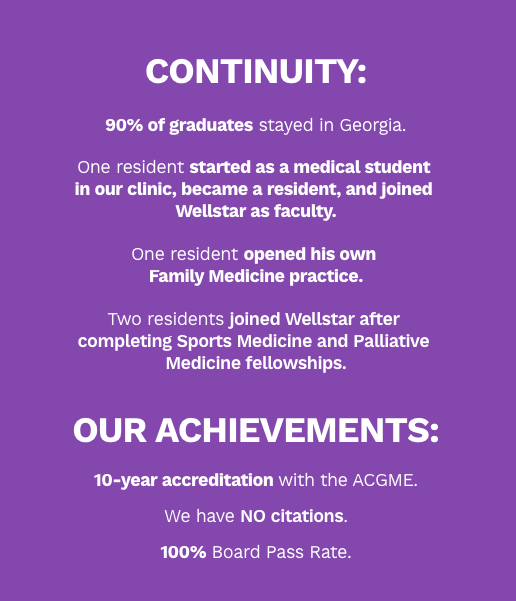
Our program is designed to offer a comprehensive and holistic approach to medical training. You will engage in a variety of clinical experiences, hands-on training, and educational opportunities that will prepare you for the challenges and joys of family medicine. Our dedicated faculty members are here to guide and support you every step of the way. We are very excited and proud to continue with our 100% board passage rate.
As a member of our program, you are not just a resident — you are a vital part of our family. Our program is not just about medical education. It’s about building lasting relationships, understanding the unique needs of diverse patient populations and embracing the values of compassion and empathy. It is so rewarding to see our graduates coming back to visit us and sharing their successes.
We encourage you to take full advantage of the resources and opportunities available to you, from our state-of-the-art facilities to our collaborative research initiatives. Our goal is to empower residents to become compassionate, skilled and well-rounded family physicians. Our graduates take care of the whole family, including pregnant patients, pediatric patients and geriatric patients. This experience allows residents to get jobs and fellowships before they graduate.
I am confident that your time in our program will be transformative, and I look forward to witnessing your growth and success. Please know that my door is always open, and I am here to support you in any way I can.
Once again, welcome to our program. Together, we will embark on a journey of learning, service and community that will shape not only your medical career but also the lives of those you will serve.

Nestled within the heart of our community, our family medicine residency program embodies the essence of camaraderie, integrity and patient-centered care. At our program, we believe in delivering world-class PeopleCare. With a focus on health equity, we strive to bridge gaps and ensure equitable access to healthcare for all by providing financial aid assistance and utilizing our advanced in-house services. Our family environment sets us apart from other programs, which allows us to nurture successful future physicians.
To be considered for a Family Medicine rotation at Wellstar Kennestone, please submit the following information via the form link:
Form Link: https://forms.office.com/r/Rb3E14LHxF
*Longitudinal rotations: 1. Behavioral Medicine longitudinal experience 2. Research and COPC (Community-Oriented Primary Care, which is a population-based approach to identifying and addressing community health concerns.
The type of research we do is clinical-based medicine and community-based medicine focusing on populations and social determinants of health.
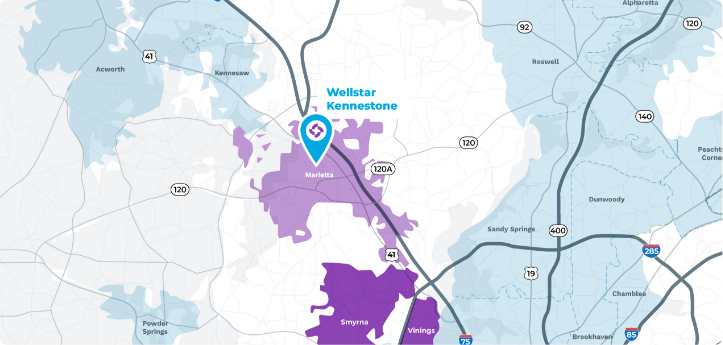
Perfectly positioned between the north Georgia mountains and the city of Atlanta, Marietta is the ideal place for young professionals and growing families. Equal parts hip and hometown, it’s a bustling city with a small-town feel.
Marietta’s historic downtown square is alive with activity, hosting regular farmers markets, concerts, and festivals. The Battery and Truist Park (home of the Atlanta Braves) provide entertainment for everyone in the Vinings neighborhood. Marietta is also a short drive to Downtown Atlanta and the Hartsfield-Jackson Atlanta Airport.

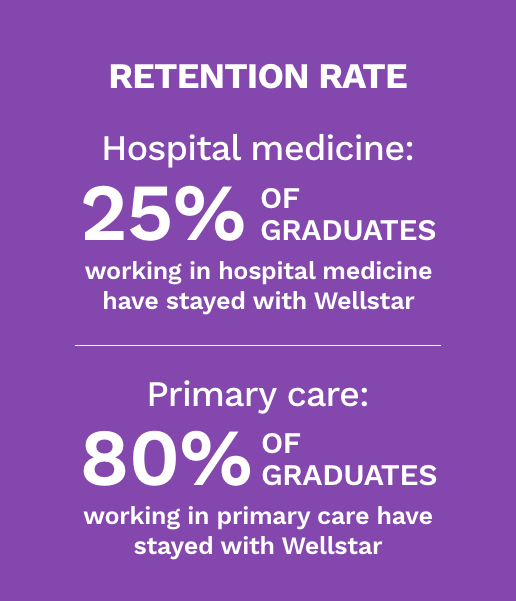
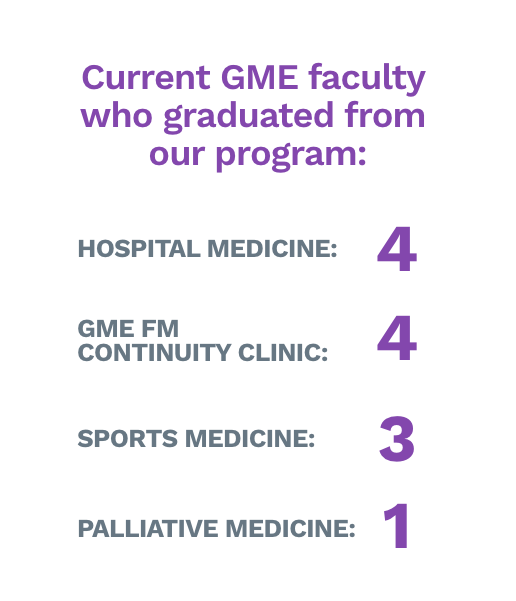
We have had graduates enter fellowships in palliative and sports medicine, become hospitalists and group practitioners (in Wellstar hospitals), and receive teaching positions.
The night before interview day, we carve out time for you to meet with our current residents, faculty, and program leadership to ask questions and hear about their experiences. On interview day, you will participate in several individual interviews as we try to get to know you as a candidate. We will also give you the opportunity to join our grand rounds during the day.
We want to get to know you as a person and learn as much as we can about your overall experience during your interviews. If you meet all application requirements, we have no preference regarding your undergraduate focus.
Family medicine residents are given academic half days every Wednesday from 1 to 5 PM. During this time, you’ll participate in board review, journal club, case reports, faculty-led academic reviews of EBM and wellness activities, among other didactics.
Yes, we have our own inpatient hospital service. Our team is made up of residents from each year (PGY1, PGY2, PGY3) and a family medicine supervising physician.
During PGY1 year, you do not take call for our inpatient service. Inpatient service call begins during PGY2 and PGY3 years. You will have approximately two to four 24-hour shifts throughout the year and two to four 12-hour shifts. Throughout all years (PGY1, PGY2, PGY3) you will take OB call for our family medicine OB service.
We understand residency is one of the most stressful and demanding periods of your medical training. We take wellness very seriously here at Wellstar Kennestone Family Medicine Program. We have “wellness Wednesday” on any fifth Wednesday of the month. During this day, you will take part in fun activities with the residents of the program. We also have a program-wide yearly retreat. Day to day we are committed to ensuring that our residents remain emotionally and physically healthy, whether that be encouraging exercise, drinking water or providing a hug.
With the guidance of our research faculty professor, residents are encouraged to do research and scholarly activities throughout all three years. You will meet once per month with your class for COPC. As a PGY2, you will participate in a group project in preventative health. As a PGY3, you will work on an individual project of your choice with the opportunity to present it at the end of the year.
Throughout each year you will meet regularly with our licensed clinical health psychologist. You will be introduced to the biological, behavioral, psychological, and social sciences relevant to health and illness. You can also take an elective in behavioral medicine.


Dr. Viktoria Nurpeisov earned her bachelor’s degree from Georgia State University in Atlanta and received her medical degree from the Medical College of Georgia. She completed her residency at Atlanta Medical Center. Her commitment to excellence led her to complete a geriatric medicine fellowship at Emory University in Atlanta, earning dual board certifications in family medicine and geriatrics.
She is a board-certified geriatrician and certified medical director of Cobb A.G. Rhodes Nursing Home. She is certified by the American Board of Family Medicine, and she is a fellow of the American Academy of Family Physicians. She also is a member of the American Academy of Family Physicians, the American College of Obstetricians and Gynecologists and the American Geriatrics Society.
She is currently in practice at Wellstar Family Medicine GME Smyrna Clinic, and she serves as the program director of Kennestone Family Medicine Residency Program.
Dr. Nurpeisov’s career is marked by numerous publications, successful grant endeavors and active participation in multiple committees. Her passion lies in stress management, group facilitation and educational programming focusing on physician well-being. Beyond her professional life, Dr. Nurpeisov enjoys deep-sea fishing, gardening and cherishing moments with her family. Her multifaceted expertise and dedication underscore a career dedicated to enhancing healthcare, educating future physicians and promoting holistic well-being within the medical community.


Dr. Guilherme Costa, a distinguished attending physician hailing from Brazil, brings a profound love for teaching medicine and a genuine nerdiness for pathophysiology. Dr. Costa completed his residency in family medicine at Wellstar Kennestone, where he also earned recognition as Wellstar 1st Place in Research 2023, Teaching Resident of the Year 2023 and Georgia Primary Care Association 1st Place in Research 2022.
With a global wanderlust, Dr. Costa and his significant other traverse the world, capturing moments through the lens of photography. Beyond the medical realm, Dr. Costa indulges in the dynamic world of stock trading and investments, all while exploring a burgeoning passion for wines. A multifaceted professional, Dr. Costa embodies a rich blend of medical expertise, cultural exploration and diverse interests.


Dr. Alan Dever is the director of research in the GME family medicine program. He earned his medical doctorate from the Medical University of the Americas, Nevis, West Indies, and earned his Doctor of Philosophy degree from the University of Michigan. Dr. Dever also earned his master’s and bachelor’s degrees from State University of New York at Buffalo. In addition, he holds an honorary degree in preventive medicine from Kanazawa Medical University, Japan, and an honorary Master of Public Health degree from Emory University.
With over 25 years of research experience, Dr. Dever has held many leadership positions with Mercer University School of Medicine in Macon and served as the founding chairman of the department of community medicine. A Professor Dean Emeritus at Mercer University, he also created and oversaw the Master of Public Health program. In addition, he is an ad hoc member of the Georgia Board for Healthcare Workforce, a member of the Steering Board for State Wide Area Health Education Centers and an advisory committee member of the Master of Public Health Program, Mercer University School of Medicine.


Dr. Maclin is a clinical psychologist and currently the behavioral health faculty for the GME family medicine residency. In that role, she functions in a multifaceted manner—clinical, teaching, supervisory and administrative. Dr. Maclin provides psychological care to patients seeking mental health services within the primary care clinic. She facilitates a didactic series for the residents to workshop behavioral medicine concepts relevant to the medical encounter. She supervises medical residents via live video stream, providing feedback on patient-provider communication. Additionally, she assists residents in research development and project construction. Dr. Maclin earned her doctoral degree in clinical psychology from the University of Memphis and completed postdoctoral training in clinical health psychology at the Atlanta Veterans Affairs Health System. Dr. Maclin is most interested in supporting systems of health equity—teaching physicians and as a clinician specializing in culturally centric integrated clinical health psychology. Dr. Maclin has published research and conference presentations that highlight the intersection of BIPOC identity and health behaviors.


Originally from New York City, Dr. Mathieu completed his family medicine residency and geriatric fellowship in Georgia. He enjoys spending time with his family and his favorite pastimes are trying new recipes, traveling and watching action sci-fi movies.


Dr. Nichols’ life story is a blend of things he really enjoys. He completed his residency in family medicine at Wellstar Kennestone, and now as faculty at Wellstar Kennestone Family Medicine, he helps shape future doctors by connecting with residents, medical students and patients—and making a difference in all their lives.
Outside the hospital, he loves embarking on road trips and exploring new places, both in the country and around the world. Whether it’s the scenic beauty of local landscapes or the excitement of international adventures, travel has become a big part of his story.
Dr. Nichols also loves spending time repairing cars which represent a mechanical heart to his experience, providing a respite from daily life events. He enjoys spending time with family, including his nieces and nephews, and his animal companions who keep him grounded.


Dr. Daroine Tekleyes, an attending physician at Wellstar GME, serves as the assistant program director and outpatient faculty, exemplifying a profound commitment to medical education and mentorship. Dr. Tekleyes went to medical school at St. George’s University and completed her residency at Atlanta Medical Center. Fluent in three languages—English, Creole and French—she effortlessly bridges linguistic and cultural divides, fostering inclusivity and understanding in healthcare.
Beyond her clinical prowess, Dr. Tekleyes is an avid traveler, embracing diverse cultures and enriching her perspective. A dedicated mother of five, she gracefully balances the demands of her profession with cherished family time, nurturing her children with love and wisdom. An ardent bibliophile, Dr. Tekleyes finds solace and inspiration in the pages of literature, while her passion for arts and crafts ignites creativity and joy.


Dr. Lucy Triana stands as a distinguished core faculty member of the Wellstar Kennestone Family Medicine Residency Program, where she also completed her residency in family medicine. A graduate of the esteemed Pontificia Universidad Javeriana in Bogota, Colombia, her journey in medicine has been marked by a dedication to excellence and service. With a background in emergency medicine, Dr. Triana honed her skills while serving with the Colombian Red Cross, embodying resilience and compassion in times of crisis.
Further enriching her expertise, she pursued pediatric studies in Seville, Spain, embracing the global exchange of medical knowledge. Beyond medicine, Dr. Triana finds joy in the great outdoors, often embarking on hiking and camping adventures with her three sons and her husband, fostering bonds and creating lasting memories.
Her commitment to the community extends to her involvement with the Boy Scouts of America Atlanta Area Council, where she imparts values of leadership and camaraderie. A multifaceted individual, Dr. Triana finds solace and expression through her hobbies of playing guitar, dancing and sharing her voice at her church. Fluent in both English and Spanish, Dr. Triana embodies a bridge between cultures, fostering understanding and connectivity in her professional and personal endeavors.


Dr. Samina Qaiser is a core inpatient faculty who has been with the program since its inception. Dr. Qaiser is actively engaged in teaching the diagnosis and management of the hospitalized patient. She participates in residents’ scholarly and research activities. She also supports the wellness of the residents on inpatient by taking the residents to lunch and making sure the residents’ wellness is preserved.




Hometown: Carolina, Puerto Rico
Medical school: University of Medicine and Health Sciences St. Kitts
Clinical interests: Procedures, global health, women’s health and emergency medicine
Personal interests & hobbies: Theology, music, fitness and yoga and cooking
Why family medicine? Because of the versatility to serve all types of patient populations in multiple settings while providing the best quality of care
Why did you choose Wellstar for your residency? It had the most supportive and collaborative staff, residents and faculty. Also, an excellent comprehensive curriculum and the best benefits.










Hometown: Honolulu, HI
Medical School: Trinity School of Medicine
Clinical Interests: Pediatrics, women’s health, procedures, sports med, Diapers to diapers and everything in between!
Personal Interests & hobbies: surfing, pickleball, snowboarding, running, climbing, & faith!
Why Family Medicine? Able to impact & care for the entire family and do such a variety!
Why Wellstar? The family med program Ohana here at Wellstar is incredible & the well rounded in-depth training we receive is what made it number one for me!!
Hometown: Canton, Georgia
Medical school: Philadelphia College of Osteopathic Medicine – South Georgia Campus
Clinical interests: Primary care, preventive medicine, and geriatrics
Personal interests & hobbies: Family, woodworking, beekeeping, hiking, and gardening (both successfully and unsuccessfully)
Why Family Medicine? Very few people have been able to make me feel as truly cared for, safe, and heard as the family medicine physicians in my life. I am humbled by the idea of being able to care for patients who trust me with being their partner in healthcare while also creating meaningful and long-lasting professional relationships.
Why did you choose Wellstar for your residency? Each and every member of the Wellstar community consistently impresses me with the effortless kindness and compassion they exhibit on a daily basis, and I am truly honored to be a part of this wonderful team.


Hometown: Port St Lucie, FL
Medical school: Ross University School of Medicine
Clinical interests: Hybrid style (inpatient and outpatient), Lifestyle medicine, Women health and Adolescent medicine
Personal interests & hobbies: Spending time with my family, working out, binge watching reality tv shows
Why Family Medicine? I chose family medicine because I want to advocate for vulnerable populations and build lasting relationships with patients at every stage of life. It’s a field where I can treat and prevent illness, stay connected to the communities I serve, and become a trusted part of a family’s support system.
Why did you choose Wellstar for your residency? During my rotation at Wellstar, I immediately felt welcomed and supported. The inclusive culture, the genuine compassion shown toward patients, and the strong sense of teamwork left a lasting impression on me—and made it clear that this was a place I wanted to come back to.


Hometown: Atlanta, GA
Medical school: Government Medical College, Patiala
Clinical interests: Women’s Health, Preventive Care, Procedures
Personal interests & hobbies: Reading, Painting, Cooking/Baking
Why Family Medicine? I chose Family medicine Holistic care, health promotion, and focus on preventive care all drew me to family medicine
Why did you choose Wellstar for your residency? From supportive culture, well -rounded curriculum to resident well-being, it felt like a place where one can grow both as a physician and a person.
Hometown: Johns Creek, GA
Medical school: Mercer University School of Medicine
Clinical interests: Family Medicine with an interest in Sports Medicine.
Personal interests & hobbies: Volleyball, Soccer, Escape Rooms, Board Games
Why Family Medicine?: Get Family Medicine is amazing because you get to see first hand the positive impact you can have on a community and the clinical diversity of patient population always keeps you learning new things. It’s not just the acute care, but also the chronic medical condition management with associated procedures that really makes every day fun.
Why did you choose Wellstar for your residency?: Between the incredible family medicine program staff/residents and Wellstar’s reputation and impact in the community, it was a no brainer. Everyone wants to work in an engaging environment with great people!


Hometown: Douglasville, GA
Medical School: Xavier University School of Medicine
Clinical Interests: Outpatient and inpatient medicine, substance abuse, and women’s health
Personal Interests & hobbies: Spending time with family and my dogs, exploring national parks and hiking, reading humorous fiction, thrillers, and fantasy fiction, and traveling.
Why Family Medicine: Family Medicine allows me to pursue my passion for health equity and my desire to care for diverse populations from all ages and walks of life, especially those traditionally marginalized by the larger healthcare system. Family Medicine as a field allows me to build meaningful long-term connections with my patients and their families while also advocating for their rights and uplifting their voices.
Why did you choose Wellstar for your residency? I remember volunteering at Wellstar during my high school years and saw early on how open and welcoming everyone was. This program embodies the values I felt were most important to me. It truly is a place where you feel compassion, supported, and a part of a family. Its an environment that allows you to grow and become a competent and well-rounded physician while learning from a diverse community of faculty and colleagues.


Hometown: Dalton, Georgia
Medical school: PCOM Georgia
Clinical interests: Preventative medicine, nutrition and wellness, dermatology
Personal interests & hobbies: Cooking, trying new foods, being outdoors, and going to sporting events
Why Family Medicine? I chose family medicine because of the continuity of care, the variety in practice, and the ability to take care of patients of all ages. I also value the focus on prevention and the holistic approach to primary care.
Why Wellstar? While rotating with the program as a medical student, I worked with genuinely kind and supportive residents, faculty, and staff. I knew then it was the right place for me to grow into the well-rounded family physician I hope to become. The location in my home state was also a major bonus!


Medical school: Ross University
Clinical interests: Global health, women’s health, pediatrics and dermatology
Personal interests & hobbies: Concerts, music festivals, traveling, and art museums
Why Family Medicine? I chose family medicine because it encompasses all of my clinical interests into one specialty. It focuses on building long-term relationships with patients of all ages and backgrounds.
Why did you choose Wellstar for your residency? I chose Wellstar because of their comprehensive training, emphasis on community health, and supportive learning environment.


Hometown: Columbus, Georgia
Medical school: Medical College of Georgia
Clinical interests: My clinical interests include primary care, women’s health, and geriatrics, with a focus on improving the quality of life. My interests extend beyond individual care into community health and global health initiatives, aiming to create sustainable health improvements on a larger scale.
Personal interests & hobbies: When not engaged in my clinical pursuits, I am a devoted cat mom, enjoy traveling, and love being outdoors, rollerblading, and biking. I enjoy volunteering, particularly serving vulnerable groups and in disaster relief efforts. My hobbies also include yoga, various art projects, and learning different mediums for my art.
Why family medicine? Family medicine stands out to me as the cornerstone of holistic and compassionate care, but also as a practice enriched by data and technology to improve care coordination. It offers the unique opportunity to form lasting relationships with patients across all ages and stages of life, addressing not just the physical aspects but the emotional and social factors that contribute to well-being. This field allows me to integrate my diverse clinical interests and make a difference in the lives of individuals and communities alike, by being the first contact for health concerns, guiding patients through the health care system, and coordinating comprehensive care.
Why did you choose Wellstar for your residency? My decision to join Wellstar for my residency was driven by the program’s strong commitment to comprehensive patient care, its supportive culture, community health, and mentorship opportunities. The program’s focus on comprehensive training, including practice management, continuity of care, and diverse patient panels align with my clinical interests and goals in serving diverse populations in outpatient settings.


Hometown: McDonough, Georgia
Medical School: Ross University School of Medicine
Clinical Interests: Women’s Health & Obstetrics, Behavioral Health, Community Medicine
Personal Interests & Hobbies: Reading, Volunteering and mentorship, cooking my favorite Caribbean foods!
Why family medicine: I chose family medicine because it allows me to do a little bit of everything in medicine, focus on primary care, and be a constant figure in my patients’ lives, from birth onwards!
Why did you choose Wellstar: The state of the art facilities, prime location in my home state, and commitment that the residents and faculty had for the program. Also, everyone I interacted with was so kind and passionate about caring for their patients and the surrounding community.


Hometown: Tallapoosa, GA
Medical school: Mercer University School of Medicine
Clinical interests: pediatrics, geriatrics, procedures, ultrasound
Personal interests & hobbies: arts & crafts, cooking/baking, pickle ball
Why family medicine? I chose Family Medicine due to the opportunity to care for and serve the entire community — from newborn to elderly! I also enjoy the ability to have an impactful role in the community and be the key leader in my patient’s overall health.
Why did you choose Wellstar for your residency? I chose this program because I felt as if it offers the best learning environment with its combination of supportive faculty/co-residents, large patient panels, diversity of clinical cases, and resident well-being. While also being close to home, I know that this program will allow me to grow and become the best physician equipped to serve the state of GA!


Hometown: Alpharetta, GA
Medical school: PCOM-GA
Clinical interests: Preventive medicine, Chronic disease management
Personal interests and hobbies: Outdoor activities, Sci-Fi/Thriller/Horror TV and Movies, Computers and Video Games, Cats!
Why family medicine? My clinical interests in preventive medicine and chronic disease management naturally led me to choose family medicine. Additionally, the combination of continuity of care, a diverse patient population, and the flexibility and versatility of family medicine is unrivaled in my opinion.
Why did you choose Wellstar for your residency? I had a very pleasant experience during my family medicine clerkship at Wellstar. Interacting with the residents and faculty showed me that they truly operate like a family, and I felt I would fit in well with the group. The location and proximity to my family and friends were also major deciding factors for me.


Hometown: Osun (Ara), Nigeria
Medical school: Windsor University School Of Medicine
Clinical interests: Women’s health, primary care, hospital medicine, Research medicine, Lifestyle, and preventive medicine.
Personal interests and hobbies: Connecting with people, reading, traveling, cooking, interior decor, shopping, makeup, and spending time with my family.
Why family medicine? Growing up in Nigeria, I quickly realized the importance of primary care in the community and believe that Family Medicine, as primary and preventive care, is one of the core essential societal pillars needed to hold and strengthen a community’s health. I aspire to assist families through various aspects of their health needs while being an advocate for them as I wholeheartedly find honor in answering the call of medicine that presents the poor and underserved, the addicted, and often the voiceless.
Why did you choose Wellstar for your residency? I chose Wellstar because I was confident that here, I would receive comprehensive training, see diverse patient populations, continue to develop my research interests and have limitless opportunities for hands-on experience. This would make me a well-rounded physician who would have a positive impact on the world. Also, I cherished the strong faculty support and their open-door policy.


Hometown: Ottawa, Ontario, Canada
Medical school: University of Medicine Health Sciences (UMHS)
Clinical interests: Sports Medicine and Lifestyle Medicine
Personal interests & hobbies: Golfing, traveling, cooking and music
Why family medicine? Family medicine’s emphasis on patient-centered care will allow me to build strong relationships with patients and help them proactively maintain their health and well-being.
Why did you choose Wellstar for your residency? Wellstar gave me a sense of community and comfort, enabling me to excel in my professional and personal growth.


Hometown: Sugar Hill, GA
Medical School: PCOM-GA
Clinical interests: Preventative care, Sports Medicine, Procedures, Community Health
Personal interests & hobbies: Tennis, Hiking, Cooking, and Watching Movies
Why family medicine? I chose to pursue family medicine to cater to an all inclusive patient population. Not only can I treat people of all ages, I can also function as a central point of care for patients who require specialized care.
Why did you choose Wellstar for your residency? The faculty support and environment at Wellstar provides an enriching inpatient and outpatient settings, which allows for residents to provide exceptional patient care.


Hometown: Lilburn, GA
Medical school: Philadelphia College of Osteopathic Medicine
Clinical interests: Integrative medicine and psych
Personal interests & hobbies: Dance, travel, food
Why family medicine? Continuity of care, breath, and focus on prevention all drew me to family medicine.
Why did you choose Wellstar for your residency? From the culture of Wellstar to the complex cases, I know this program offers an unparalleled learning experience.


Hometown: Snellville, GA
Medical school: Philadelphia College of Osteopathic Medicine–Georgia Campus
Clinical interests: Geriatrics and palliative medicine
Personal interests & hobbies: Painting, reading and spending time with family
Why family medicine? I chose family medicine because of its wide scope. It’s a field that ranges from cradle to grave and everything in the middle. I love being able to help out anyone from my community.
Why did you choose Wellstar for your residency? I chose Wellstar Family Medicine because of the amazing team! Everyone is very welcoming and kind.


Hometown: Carolina, Puerto Rico
Medical school: University of Medicine and Health Sciences St. Kitts
Clinical interests: Procedures, global health, women’s health and emergency medicine
Personal interests & hobbies: Theology, music, fitness and yoga and cooking
Why family medicine? Because of the versatility to serve all types of patient populations in multiple settings while providing the best quality of care
Why did you choose Wellstar for your residency? It had the most supportive and collaborative staff, residents and faculty. Also, an excellent comprehensive curriculum and the best benefits.


Hometown: Orlando, Florida
Medical School: Ross University
Clinical Interests: Preventive medicine, women’s health and global health
Personal Interests & Hobbies: Hiking, traveling, exploring diverse cuisines and spending quality time with family
Why family medicine? I chose family medicine for its versatility across all ages and my passion for preventive care.
Why did you choose Wellstar for your residency? I chose Wellstar Kennestone because the program promoted a close-knit, family-like environment, fostering strong connections and support among the team.


Hometown: Valdosta, GA
Medical school: Philadelphia College of Osteopathic Medicine–Georgia Campus
Clinical interests: Women’s health, global medicine, nutrition/wellness, proceduresand osteopathic manipulative medicine
Personal interests & hobbies: Hiking, traveling, cooking, gardening and watching documentaries and learning more about the world around us
Why family medicine? Family medicine allows me to take care of the entire family, from bringing life into the world to comforting those about to leave the world. Family medicine physicians have the capacity to do a little bit of everything and become intertwined in a patient’s life. In family medicine, I can create the practice that can impact a community from being on the front line of healthcare to helping coordinate patients’ care.
Why did you choose Wellstar for your residency? Wellstar is a place that values its members and takes pride in caring for patients. I chose Wellstar because I felt right at home from the beginning. Having several friends in medical school complete residency at Wellstar, I only heard good things. The leadership caters to each resident and allows the residents to explore their interests.


Hometown: Damascus, GA
Medical school: St. George’s University
Clinical interests: Sports medicine, nutrition and longevity
Personal interests & hobbies: CrossFit, history and podcasts
Why family medicine? Family medicine offers flexibility in career choices and the opportunity to care for patients’ lives beyond the clinic and hospital.
Why did you choose Wellstar for your residency? For its genuinely welcoming interview experience and robust clinical rotations.


Hometown: Fayetteville, GA
Medical school: University of Health Sciences Antigua School of Medicine
Clinical interests: Integrative medicine
Personal interests & hobbies: All things self-care
Why family medicine? I chose family medicine because I enjoyed the patient-centered approach to care and the unique physician-patient relationships/longitudinal relationships. Family medicine offers a wide range of practice in multiple settings, which allows me to tailor future practice to my specific interests.
Why did you choose Wellstar for your residency? Because of the diversity of the program and the supportive and nurturing environment.


Hometown: North Port, Florida
Medical school: Philadelphia College of Osteopathic Medicine
Clinical interests: Geriatrics
Personal interests & hobbies: Powerlifting, movies/anime, learning new cooking recipes and video games
Why family medicine? I chose family medicine because it allows me to practice on a broad demographic of patients. I find myself passionate in the continuity of patient care and being able to meld personal life in coordination with patient care.
Why did you choose Wellstar for your residency? This program provides me a safe and supportive platform to grow as a well-rounded physician. In addition, the team I work with challenges me to be the best colleague and physician for the patient population.


Hometown: Bronx, New York
Medical school: Philadelphia College of Osteopathic Medicine
Clinical interests: Dermatology and geriatrics
Personal interests & hobbies: Kayaking, weightlifting and day trading
Why family medicine? I chose family medicine because of all the specialties; I believe we see the most diverse pathology and age groups. From AFib to zoonotic, we see it all.
Why did you choose Wellstar for your residency? I chose Wellstar because it’s a friendly and encouraging environment for learning. Our preceptors are great—in and out of the hospital. The cafeteria allowance didn’t hurt either.


Hometown: Millbrae, California
Medical school: Windsor University School of Medicine, St. Kitts & Nevis
Clinical interests: Hospital medicine and full-scope outpatient medicine
Personal interests & hobbies: Cars and motorcycles, hiking, cooking and aquariums
Why family medicine? As a medical student, I enjoyed aspects of every specialty I rotated under. It was by the end of my rotations that I realized I wanted to practice a broad scope of medicine in various clinical settings. Family medicine was the natural choice for me.
Why did you choose Wellstar for your residency? Wellstar is a large health system that offers many resources for my patients, including financial assistance, and all the specialists and services I would need to provide comprehensive care to my patients in both the outpatient and inpatient setting.


Hometown: Naperville, Illinois
Medical school: University of Medicine and Health Sciences, St. Kitts
Clinical interests: Outpatient care, children, adolescents, adults and procedures
Personal interests & hobbies: Dance, hiking, biking, traveling, spending time with my husband, our daughter and our golden lab mix, baking, finding new places to eat (especially bakeries, cafes and coffee shops) and finding new ways to stay active
Why family medicine? I really enjoy continuity of care and having the opportunity to learn about a variety of conditions.
Why did you choose Wellstar for your residency? The previous years always spoke very highly of the program, the people and the opportunities. I knew I would receive high-quality training by choosing this program. The most important reason—the residents and faculty are always happy.


Hometown: Baton Rouge, Louisiana
Medical school: Morehouse School of Medicine
Clinical interests: Women’s health and ambulatory medicine
Personal interests & hobbies: Couponing, online shopping, fishing and hunting
Why family medicine? I chose family medicine because of the variety and continuity—it is not what can a family medicine physician do, it’s what can’t they do.
Why did you choose Wellstar for your residency? The people. Everyone that I have met at Wellstar has been genuinely kind, especially the program director. Also, Wellstar offers great pathology and a plethora of specialties to learn from within the system.


Hometown: Marietta, GA
Medical school: Army Medical College, Pakistan
Clinical interests: Full spectrum family medicine, including procedures and dermatological procedures
Personal interests & hobbies: Art, reading, horseback riding, writing, travel, cooking and trying all the world cuisines
Why family medicine? I love how family medicine can help you offer comprehensive care to your patients, and how important it is to have a good PCP in your corner!
Why did you choose Wellstar for your residency? I have never seen a residency that literally is the definition of teamwork. The relationships I have fostered here are lifelong and that makes for a great learning experience!
Hometown: Duluth, GA
Medical school: Philadelphia College of Osteopathic Medicine–Georgia Campus
Clinical interests: Geriatrics
Personal interests & hobbies: Swimming, hiking, playing ping pong and building Legos
Why family medicine? I get to grow old together with my patients.
Why did you choose Wellstar for your residency? The people and the vibe


Hometown: Durham, North Carolina
Medical school: St. George’s University, Grenada, WI
Clinical interests: Integrative medicine and preventive health
Personal interests & hobbies: Hip hop dancing, hanging out with family and friends and cooking
Why family medicine? I chose family medicine for the continuity of care and to be a person’s first line of defense. I wanted to have the ability to guide and improve a person’s health, preventing fatal diseases. I love staying broad in my knowledge and love the ability to treat every age group or treat every family member.
Why did you choose Wellstar for your residency? I chose Wellstar for the camaraderie, the support system, the fact that wellness is a priority and the location.
Hometown: Sandersville, GA
Medical school: Morehouse School of Medicine
Clinical interests: Preventive and integrative medicine
Personal interests & hobbies: Gardening and cooking
Why family medicine? To build lifelong relationships with patients
Why did you choose Wellstar for your residency? To be close to family and for the supportive culture of the program


Hometown: Delmas, Haiti
Medical school: Universidad Tecnologica de Santiago (Santo Domingo Campus)
Clinical interests: Hospital medicine, adolescent medicine, sports medicine, geriatrics and women’s health
Personal interests & hobbies: Spending time with friends and family, watching reality shows and sports, reading, traveling and playing soccer and basketball
Why family medicine? Family medicine is the only specialty that gives me the opportunity to remain connected with the core aspect of medicine and allows me to provide broad spectrum care with a patient-centered approach through genuine professional connection.
Why did you choose Wellstar for your residency? Residency is a core aspect of a physician’s personal and professional development. Achieving such a goal in a diverse and astonishing institution with state-of-the-art care is key for a successful career. I strongly believe that Wellstar is the right place to help me be every patient’s dream provider.
Hometown: Kennesaw, GA
Medical school: Medical College of Georgia at Augusta University
Clinical interests: Outpatient medicine and behavioral health
Personal interests & hobbies: Soccer, puzzle enthusiast, traveling, TV show consumer and proud caretaker of one calico cat
Why family medicine? I loved the aspect of continuity of care and am interested in bridging the gap between my community and healthcare and would like to play an essential role in public health crises.
Why did you choose Wellstar for your residency? I did an away rotation during medical school and witnessed the awesome interaction between co-residents and attendings. Everyone was so welcoming and felt like family. I also wanted to stay within the metro Atlanta area.
Hometown: Houston, Texas
Medical school: Philadelphia College of Osteopathic Medicine–Georgia Campus
Clinical interests: Preventive care and palliative medicine
Personal interests & hobbies: Traveling, jigsaw puzzles and binge watching TV shows
Why family medicine? Family medicine gives you the foundation to treat patients from all stages of life, including pediatrics, obstetrics and geriatrics.
Why did you choose Wellstar for your residency? During my rotation here as a medical student, I was impressed by the supportive, collaborative environment amongst the residents, faculty and staff members.


Hometown: Miami, Florida
Medical school: Edward Via College of Osteopathic Medicine
Clinical interests: Adult and pediatric patient population, outpatient clinic experiences and in-clinic procedures
Personal interests & hobbies: Enjoying time with family and friends, hiking, gardening and cooking
Why family medicine? Family medicine allows me to care for patients of all ages and demographics and provides the opportunity to practice preventive care and maintain continuity of care through it all.
Why did you choose Wellstar for your residency? From the robust clinical pathology and various learning opportunities to the overall supportive culture, Wellstar Kennestone Family Medicine Residency Program was the perfect fit for me. It has allowed me to pursue my interests and facilitated me to provide care to patients of all backgrounds, taking into consideration their determinants of health.
Hometown: McDonough, GA
Medical School: Philadelphia College of Osteopathic Medicine–Georgia Campus
Clinical interests: Preventive medicine in general, musculoskeletal, continuity and pediatrics
Personal interest and hobbies: Weightlifting, playing sports, doggos, gaming, comedy, DBZ and family and friend time
Why family medicine? I have wanted to practice family medicine ever since high school due to inspiration from my father who has been practicing family medicine in Stockbridge, Georgia, for over 30 years.
Why did you choose Wellstar for your residency? I chose Wellstar after rotating through as a fourth-year medical student. I was so impressed with the energy from the residents and attendings. They treated each other, patients and me so well. They seemed to truly enjoy teaching me. I felt comfortable and excited to go to my rotation each day.


Hometown: Lawrenceville, New Jersey
Medical school: Philadelphia College of Osteopathic Medicine–Georgia Campus
Clinical interests: Women’s health and pediatrics/adolescents
Personal interests & hobbies: Outdoor activities (sports, hiking), traveling, entertaining and cooking for family and friends and creating new cuisines and trying new recipes
Why family medicine? I chose family medicine because I want to be a part of a team that provides care to all ages, ethnicities and socioeconomic backgrounds. I want to create long-lasting connections, instill hope and provide my patients with the push they need to thrive.
Why did you choose Wellstar for your residency? I chose this program because of the positive culture and endless opportunities for growth. We truly are one big family who care for one another.
Hometown: McRae, GA
Medical school: University of Medicine and Health Sciences at St. Kitts
Clinical interests: No particular area
Personal interests & hobbies: Kayaking, hiking, wine and reading about new science and tech
Why family medicine? I enjoy developing relationships and continuity of care.
Why did you choose Wellstar for your residency? The people and culture! I could not ask for a better group of people to work with.
Marietta Square | Truist Park | The Battery | Gone With the Wind Museum | Earl and Rachel Smith Strand Theatre | New Theatre in the Square | Ghosts of Marietta Tour | Marietta Square Farmers Market | Hilton Atlanta-Marietta Hotel & Conference Center | Cobb Galleria Centre
Cycling is a popular form of transportation in Marietta. The area is also served by the CobbLinc bus service that connects to MARTA — Atlanta’s light rail and bus network. Drivers also have quick access to I-75 and I-285 to get anywhere they need.